Everyone deserves equal access to medical care. Unfortunately, the LGBTQ+ community faces discriminatory barriers to healthcare — both personal (like stigma, stereotypes or prejudice) and institutional (like difficulty getting insurance coverage or finding physicians trained in LGBTQ+ needs). These disparities prevent LGBTQ+ people from receiving essential care, like PrEP/PeP, hormone replacement therapy, and standard cancer screenings.
According to the National Academies of Sciences, Engineering, and Medicine, a lack of clinically and culturally responsive healthcare providers remains a major concern for LGBTQ+ patients. This shortage is one of the major causes of inequality. When patients can’t find doctors that are understanding of their identity or trained in their needs, their care will suffer.
But it doesn’t have to be this way.
Let’s explore why the status quo isn’t working for everyone — and how we can fix it by providing culturally competent care.
What is Culturally Competent Care?
Cultural competence is the ability of providers and organizations to effectively deliver health care services that meet the social, cultural, linguistic, and medical needs of patients.
Cultural competence is especially important for people who belong to multiple marginalized groups. When providers are conscious of how different aspects of a person’s identity (such as race, class, gender, religion, and sexuality) overlap, they can deliver more nuanced and effective health care. This concept is known as intersectionality, and it is a key component of culturally competent care.
For example, PrEP only reduced rates of HIV transmission among white gay and bisexual men because Black and Latino men face discriminatory personal and institutional barriers that white men do not — such as increased stigma, higher rates of poverty, and lower rates of health insurance. This intersectional analysis is the first step to ensuring equal access to PrEP and creating a culturally competent healthcare system.
How to Provide Culturally Competent LGBTQ+ Care
The Personal: Ending Discrimination at the Doctor’s Office
Getting care is intimate, vulnerable, and sometimes even scary — especially for marginalized communities.
Compared to 15% of non-LGBTQ+ adults, 1 in 3 LGBTQ+ adults say they have been treated poorly by a healthcare provider. This stat includes explicit prejudice, like being refused health care because of their sexual orientation. Additionally, almost 3 in 10 transgender people have been told that providers would not see them because of their gender identity.
When LGBTQ+ people do see a doctor, their providers’ personal stigmas can lead to misdiagnosis. Case in point: Many studies show that cis lesbians receive fewer pap tests than heterosexual ciswomen, because physicians assume they are at a lower risk of cervical dysplasia because they don’t have sex with cismen. This myth has real life consequences: it puts cis lesbians at a higher risk of cervical cancer. We can also look at “trans broken arm syndrome”, a phenomenon where doctors attribute any trans patient’s health issues to their gender transition. In a recent study, nearly one-third of trans/gender-nonconforming patients reported experiencing gender-related medical misattribution by their providers.
This vicious cycle means LGBTQ+ patients are less likely to come in for checkups, less likely to receive preventive care, more likely to wait for symptoms to worsen before seeing a doctor, and more likely to be misdiagnosed.
We can break this cycle with cultural competence. When health care professionals practice cultural competence interpersonally by respecting their patients’ gender identity, chosen name, pronouns, and romantic and sexual preferences, they are laying the groundwork for a strong provider-patient relationship — proven essential for better health outcomes. In other words, the first step in treating LGBTQ+ people well is to treat them well. To deepen their intersectional understanding of LGBTQ+ health needs and barriers to care, practitioners should also stay informed on the latest research and seek out LGBTQ+ specific training — like these resources, webinars, and courses provided by the National LGBTQIA+ Health Education Center.
{{blog-image}}
The Institutional: Challenges to LGBTQ+ Healthcare
When heterosexuality and cisgenderism is treated as the norm, the needs of other communities fall through the cracks. This institutional ignorance shows up in health insurance and medical school, creating structural barriers that prevent LGBTQ+ people from getting the care they need.
Health insurance companies often deny coverage to trans/gender-nonconforming people based on ignorant and incorrect binary understanding of bodies — like denying pap smears for transgender men with intact cervixes because “only women need cervical cancer screenings.” Furthermore, intersex people make up 1.7% of the population, but their bodies are excluded entirely by the erroneous belief in a fundamental sex/gender binary.
Medical schools are also failing to prepare their students to care for LGBTQ+ patients. On average, medical students receive under 5 hours of training on LGBTQ+ issues in their entire medical education — and that has consequences. In particular, 50% of transgender patients have had to teach their providers about gender-affirming care. That means 50% of trans people are receiving low-quality care from providers they don’t (and can’t) trust.
To fight institutional barriers, we need to reimagine the entire health care system to be culturally competent. LGBTQ+ inclusion cannot be an afterthought. Health insurance companies can practice cultural competence by proactively considering different genders, sexes, and sexualities instead of making blanket decisions that endanger marginalized people. Medical schools can provide their students with comprehensive, culturally competent education on LGBTQ+ needs — such as puberty blockers, which reduce suicidality in trans and nonbinary youth by around 70%. By giving upcoming doctors adequate training on gender affirming care, we’re empowering them to do what every doctor sets out to do: save lives.
Culturally Competent LGBTQ+ Health Care is the Future
Significant strides have been made towards creating a more equitable health care experience for the LGBTQ+ community.
In 2014, the Association of American Medical Colleges asked 158 U.S. and Canada medical schools to provide LGBTQ+ inclusive curriculum to their students — and some of those schools have made great progress in the decade since. More doctor’s offices than ever are allowing patients to self-identify with their correct gender, chosen name, and pronouns. In May 2024, the Human Rights Campaign reported that health care facilities nationwide were “making significant strides” in delivering in LGBTQ+ inclusive care.
With more people identifying as LGBTQ+ than ever, it’s never been more important to embrace culturally competent care and bring on a new era of equality. Who’s with us?
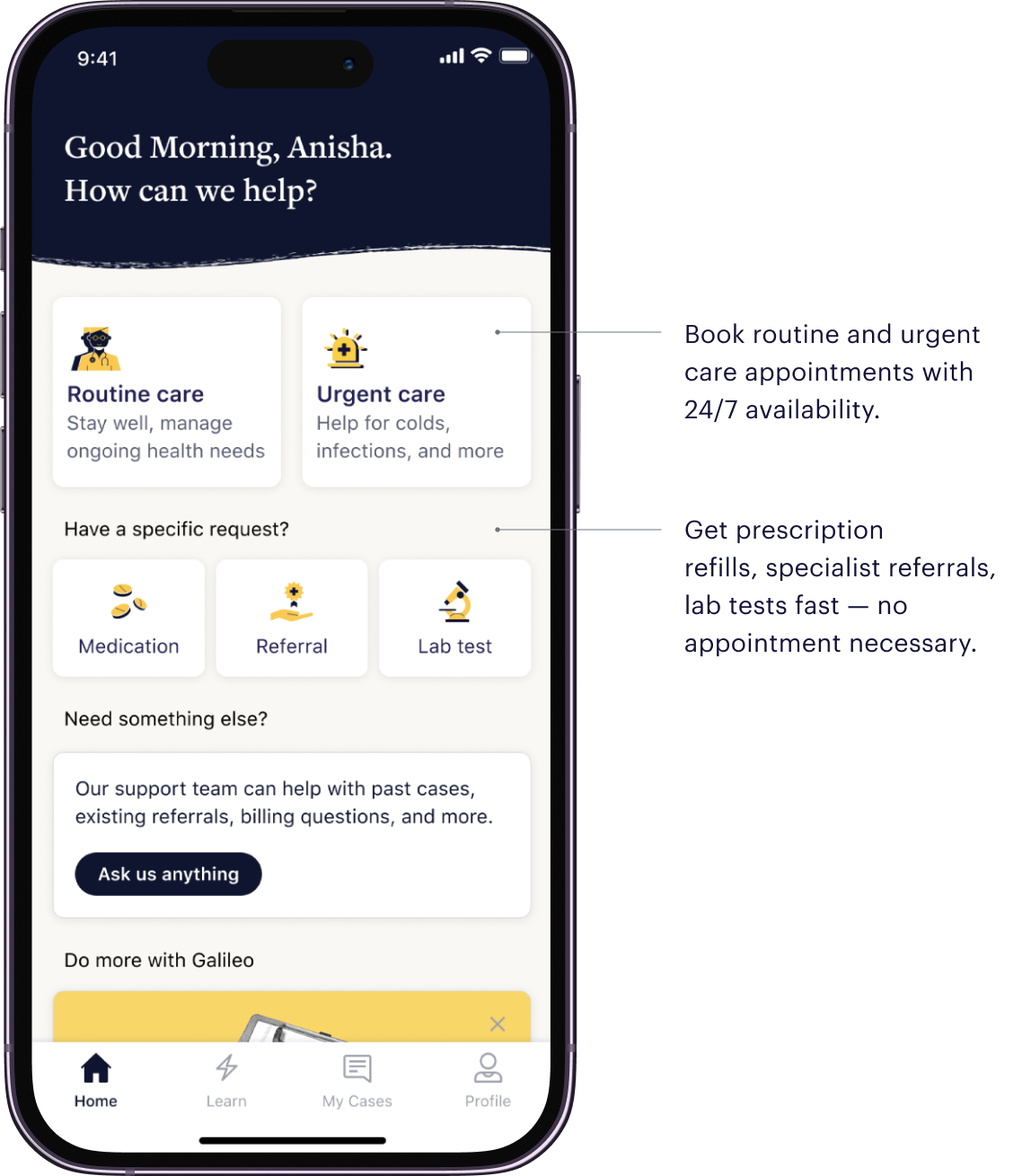
At Galileo, we make it easy to access necessary services (like PrEP/PEP), get gender-affirming care, and see culturally competent providers whenever fits your schedule.
Book your appointment today.

%20(1).webp)











.webp)