The traditional primary care model was designed to offer a longitudinal, holistic, and affordable approach to health care. Working well, it keeps overall spending low and quality of care high. But the medical climate is changing for the worse. Primary care providers in the U.S. are overbooked and overworked, with the average wait time to see a PCP is 21 days for acute or chronic illnesses. A new model of PCP care is needed, especially in today’s diverse, complex world. Here’s how employers can offer modern primary care and reduce downstream spending.
The impact of an inefficient traditional primary care system
What was once a patient-centric field is now quite disconnected. Only about a third of all care providers are PCPs, and they’re doing about half the work of all providers in the U.S.. From rushed appointments to misdiagnosis, here’s a breakdown of how it’s affecting your bottom line.
Declining availability
We’re seeing a nationwide shortage of PCPs. U.S. health care spending on primary care, in general, is falling, which is leading to fewer graduating in primary care. Many private practices today are also getting purchased by hospital systems or private equity, which often leads to higher costs of care. This means when patients seek a primary care appointment, not only are they met with long wait times or providers who aren’t taking new patients, they’re also faced with expensive premiums.
Reliance on specialists
Because PCPs are usually overbooked and have limited time with patients, they lean on specialist referrals to continue patient care. Specialists are great resources because they have knowledge that a PCP can’t have about everything. About 80% of referral diagnoses changed once a specialist stepped in. However, they don’t look holistically at a patient and only consider their area of expertise. For a patient, being bounced from specialist to specialist can lead to a lot of confusion and low quality of care. For employers, it can lead to costly tests and visits.
ER overutilization
The Emergency Room serves a specific and much-needed purpose, but it’s expensive if used outside of its scope of care. In fact, it’s about 12 times more expensive to get care at the ER for PCP-treatable conditions. And with the national shortage of PCPs, about a third of Americans get primary care from urgent care centers or the ER instead of waiting for a PCP appointment. The ER isn’t designed to provide longitudinal holistic care, like follow-ups or specialized knowledge. Over time, this habit can lead to high costs and low quality of care.
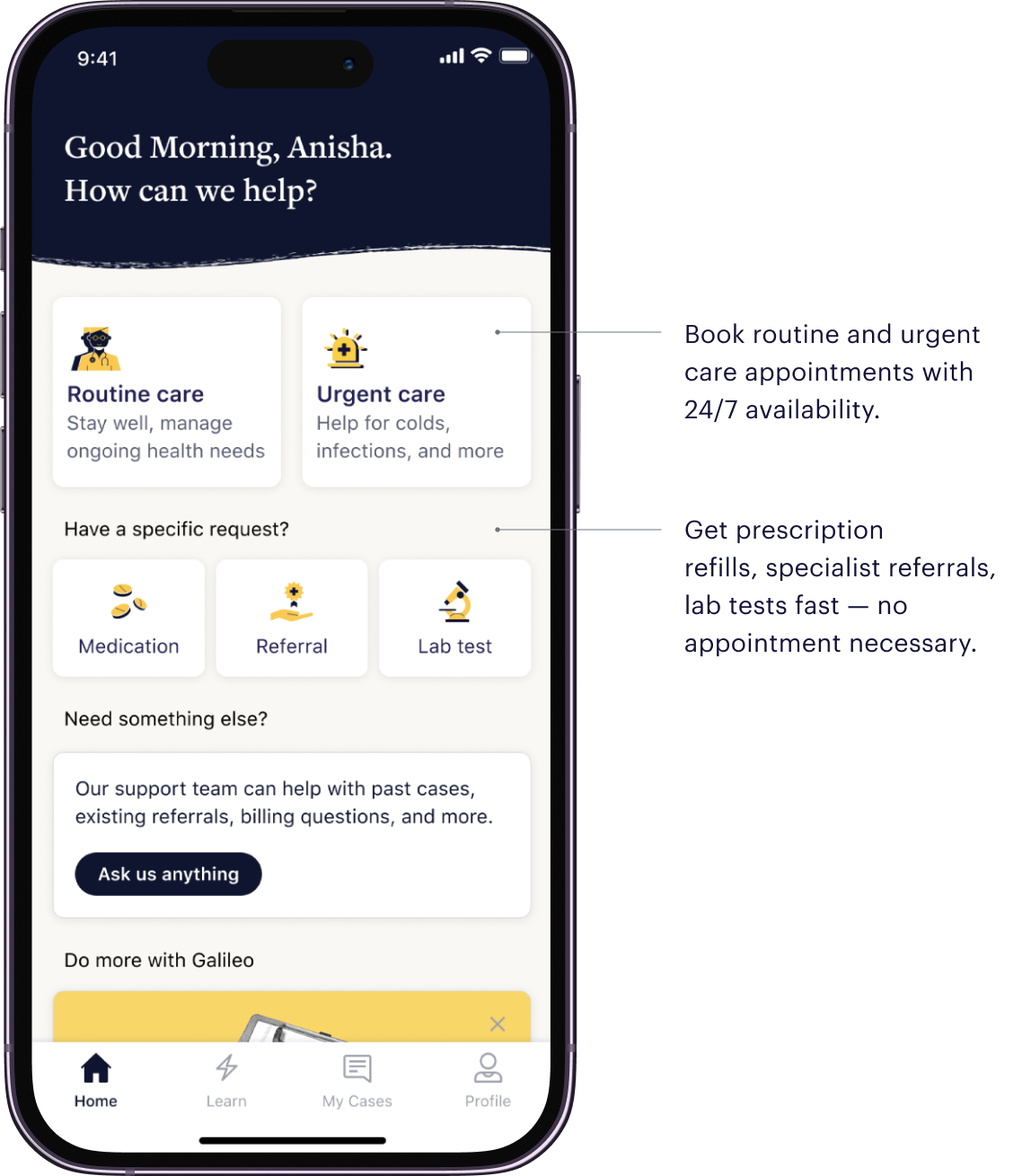
An improved, integrated care model
Primary care needs an overhaul, and it starts with an integrative approach that incorporates primary care, urgent care, and specialized care, all in one place. At Galileo, we remove the responsibility of treating hundreds of patients from a single provider. Instead, our team of multidisciplinary providers, backed by clinical decision-making tools, work together on patient cases.Collaborative care allows providers to focus on preventive care and address multiple health issues simultaneously, increasing in-house treatment success and reducing the need for costly external referrals. A modern care model like this leads to 87% of care resolved without a referral and an 11.5% reduction in the total cost of carefor employers.
The current primary care system is struggling. Offering quality primary care helps close gaps in health care by preventing high-cost chronic conditions and hospital visits. In fact, every $1 increase in primary care spending produces $13 in savings. Galileo is designed to overcome the barriers that traditional PCPs face today. Reduce downstream spending and improve the quality of care you offer employees.

%20(1).webp)












.webp)